Paravertebral hypertonicity has been documented in Chiropractic, Orthopedic
and Osteopathic literature.1 Muscular tension has been noted upon physical
examination of the spine to be associated with spinal misalignment, dysfunction
and instability. These observations have often been anecdotal
and incidental to other more objectifiable findings. It is
most often assumed that the hypertonicity, even when found on only one
vertebral level, represents spasm. The inference is that continued
muscular activity while the subject is at rest must be a pathological or
a "facilitated state."2 That this activity is segmental in nature
has only rarely raised suspicion as to the nature of such a localized
spasm. It has gone almost without question that the "spasm"
is causally related to the subluxation. Further, even when
authors have suggested the reverse (i.e., that the muscle is an effect
of the subluxation), they still often argued that this muscle activity
is counter-productive. It is my contention that resting segmental
muscular activity is homeostatic in nature. The muscles of
the spine represent the active stabilization for the functional spinal
unit.3,4 A disturbance in the three-joint complex stimulates proprioceptive
neural sensory impulses that apprise the spinal cord and subcortical brain.5
The central nervous system could then stimulate guarding muscular action,
seeking to reestablish functional balance. This phenomenon may take
place often and be involved whenever there is a difference between the
actual and intended movement or position of a functional spinal unit.6,7
In this way resting activity of the muscles would be physiologic and protective
in nature. The mechanism which is thought to underlie such behavior
is the stretch reflex.8 The muscles may be serving to return the
misaligned segment to its "normal" position. Such subtle muscle
activity would also serve to alert the examining Doctor of Chiropractic
as to the existence of the dysfunctional segment. Presupposing
the predictive value of this hypothesis and the accuracy of the palpator’s
assessment, this method would also have value in determining the proper
line of force application for the adjustment. The purpose of
this study was to understand paravertebral muscular activity and its ability
to accurately predict misalignment patterns.
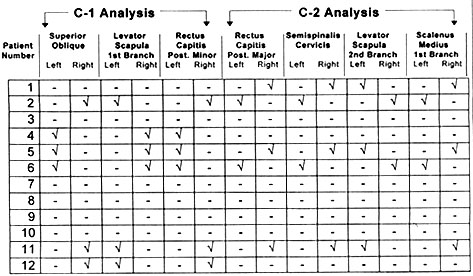
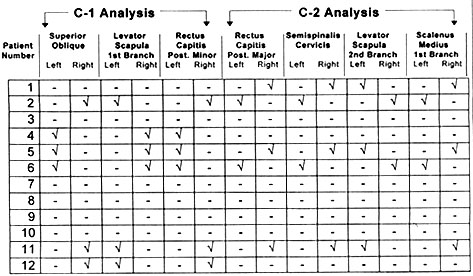
Palpation was limited to the small paravertebral muscles of the two
upper cervical vertebrae (see Table 1 ). Examination was done with
the subject supine, with the head in a neutral position, in which the muscles
were assumed to be at rest.
|
|
| · Superior oblique |
| · Levator scapula (first branch) |
| · Rectus capitis posterior minor |
| · Rectus capitis posterior major |
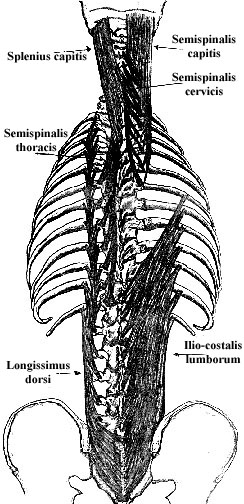
| · Semispinalis cervicis |
| · Levator scapula (second branch) |
| · Scalenus medius |
|
|
Resting muscles tension was discriminated from normal muscle tone during static palpation. This assessment was then interpreted according to the untested predictive value of this tension to discern abnormal joint position (e.g., articular dysrelationships). The anatomical relationship of the muscles to the vertebral motion segments and the theoretical muscular response to the suspected subluxation were assumed from the author's personal publication. Therefore, palpatory conclusions were derived consistent with the typical muscle pattern activity models described by the author.8 This analysis resulted in a descriptive designation of the direction of malposition for the involved segment, commonly called "listings." The listing abbreviations used by the examining doctor were simplified into four categories and are described in Table 2.
|
|
|
|
|
|
|
|
The findings were then recorded before the examiner had any knowledge of the previous radiographic findings. Radiographic interpretation resulted in listing the involved level of the spine according to the Grostic upper cervical method.
The Palmer listing system describes the anterior and superior (in reference to the relative position of the anterior tubercle of the atlas vertebra) malposition of C-1; thus, "A" is the first letter and "S" (is often) the second to designate a C-1 listing. "L" or "R" is used for describing the X-axis translation of left or right. "A" or "P" may be appended as the last letter to define possible C- 1, Y-axis rotation. These are comparative "movements" of malposition relative to the opposing side of the same segment.
This study was limited not only to the upper cervical spine but was
also focused on translation in the transverse plane. Therefore, palpatory
examination was restricted to those muscles thought to demonstrate C-1
translation of left or right and did not take into consideration the muscles
that might be used to evaluate the atlas for rotation about the Y axis.
Grostic listings included rotational findings as these findings were obtained
prior to and not exclusively for the purposes of this comparison.
Excluding disc involvement (of which the atlas has none), facet effusion
is also likely to imbalance C-1 function and set the stage for improper
loading of the opposing facet and therefore fixation. Misalignment
of the articular structures is an inevitable result of spinal column short
segment buckling, due to mechanical derangement of the connective tissues,
including deformation of the articular surfaces (e.g., collagen/proteo-glycan
gel matrix of the disc or facet cartilage).10,15 The implication is that
fixation represents an inability "...for the vertebral motor units to keep
in step with surrounding vertebrae..." or "come to rest naturally in any
given posture."8 Thus, buckling can take place gradually with successive
"cyclic or vibrational loading conditions...," but ultimately, "...the
unstable Functional Spinal Unit is characterized by a decrease in stiffness
and a resultant increase in motion under load; both the quantity and quality
of spinal motions are altered; the buckling motion appears to occur faster
than the muscles can respond..."10 Subsequent to any initial failure of
the muscles to prevent the misalignment, it seems reasonable to assume
a muscular response to a functional spinal unit (i.e., buckled).
It is likely that resting, segmental muscular activity is a response to
mechanical stretch and derangement from the vertebral malposition.
The muscular guarding may be an attempt to reestablish facet and therefore
vertebral position. Where a distinctive "rest position"15 has not
been recognized by research, it is undeniable that functional efficiency
would demand that the vertebrae articulate according to the dictates of
neural expectations. The central nervous system employs reflex mechanisms
to maximize the performance of subordinant structures.5 The stretch reflex
is the dominate controlling factor of the musculoskeletal system16 and
sets precise neural parameters with structural and functional considerations.
Concerning vertebral placement, only the muscle spindle can generate segment
specific activity, whereas most of the other stimuli arise from afferent
receptors which ultimately communicate polysynaptically with the paravertebral
muscles."17,18 Although Kirkaldy-Willis equivocates on the subject of cause
and effect, reflex, segmental muscular activity in the resting spine can
be thought to guard the affected tissues of the dysfunctional segment.
He notes that "The posterior segmental muscles protect the joint by sustained
hypertonic contraction."19
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
REFERENCES
1 Denslow, J. S., Clough G H, "Reflex activity in the spinal
extensors," Journal of Neurophysiology, V. 4:1941; 430- 437.
2 Denslow, J. S., Hassett C C, "The central excitatory state
associated with postural abnormalities," Journal of Neurophysiology, V.
5:1942; 393-402.
3 Dupuis, P.R., "Radiologic diagnosis of degenerative lumbar instability,"
Spine 10, No. 3:1985; 262-276.
4 Donisch, E. W., Basmajian J V, "Electromyography of deep back
muscles in man," American Joumal of Anatomy, 133: 26-36.
5 Cohen, H., Neuroscience for Rehabititation, J B Lippincott Company,
Philadelphia 1993.
6 Mains, R. E., Soechting J F, "A model for the neuromuscular response
to sudden disturbances," Journal of Dynamic Systems, Measurement, and Control,
December: 1971;1.
7 Wright, J. "Mechanics in relation to derangement of the facet
joints of the spine," Archives of Physical Therapy,1944; 201-206.
8 Spano, N., The Innate Biomechanics of the Spine. Self published,
l984.
9 Grostic, J. D., Grostic Procedure Notes. Self published,1993.
10 Weinstein J. N., Wiesel S W, The Lumbar Spine, 614- 618, W
B Saunders Company, Philadelphia 1990.
11 Panjabi, M. M., Krag, M. H., Chung, T. Q., " Effects
of disc injury on mechanical behavior of the human spine," Spine, V.
9, No. 7 1984; 707-713.
12 Jayson, M. I. V., The Lumbar Spine and Back Pain, Churchill
Livingston, New York,1987; 51, 373.
13 Gertzbein, S. D., et al, "Centrode patterns and segmental
instability in degenerative disc disease," Spine, V.10, No. 3,1985;
257-261.
14 Kirkaldy-Willis, W. H., "The relationship of structural pathology
to the nerve roots," Spine, V. 9, No.1,1984; 49-52.
15 Haldeman,S., Principles and Practice of Chiropractic, Appleton &
Lange, Norwalk, CT,1992; 248-251.
16 Grieve, G. P., Modem Manual Therapy of the Vertebral Column,
Churchill Livingstone, New York,1986; 500.
17 Wyke, B., "The Neurological Basis Of Thoracic Spinal Pain," Rheumatol
Phys. Med., V.10,1970; 356-367.
18 Schafer, R.C. Basic Principles of Chiropractic, The American
Chiropractic Association, Arlington, VA, 1990; 270.
19 Kirkaldy-Willis, W.H. Burton C V Managing Low Back Pain, Churchill
Livingstone, New York, 1992.
I would like to thank Dr. John Grostic and Life Chiropractic College, for the use of their research facility and cooperation. I would also like to thank the students of Life Chiropractic College who participated in the study.